CERVICAL CANCER

Overview and Definition
Cervical cancer is cancer that begins in the cervix, the lower, narrow part of the uterus or womb. It happens when the body’s cervical cells divide rapidly and grow out of control. These extra cells form what is known as a tumour.
Cervical cancer happens most frequently in women 30 years or older, but all women are at risk.
Causes
Most cases of cervical cancer are caused by a high-risk type of the human papillomavirus (HPV). HPV is a virus that is passed from one person to another through genital contact, such as vaginal, anal, or oral sex. The majority of women are able to fight off an HPV infection, however, at times, HPV can lead to cancer of the cervix.
Other factors that may increase the risk of developing cancer following a high-risk HPV infection include:
- Smoking
- Having an human immunodeficiency virus (HIV) infection or reduced immunity
- Taking birth control pills over an extended period of time (more than five years)
- Having given birth to three or more children
Symptoms

Initially, cervical cancer may not produce any symptoms. However, at a later stage of the cancer, pelvic pain or vaginal bleeding may occur. Although these symptoms may not always be caused by cervical cancer, the only way to be sure is for you to consult your doctor.
Often, there is a lapse of several years before normal cells in the cervix become cancerous. Abnormal cells in the cervix can be detected through a Pap test and you could also take an HPV test at the same time. If any of your results are deemed abnormal, you may be asked to undergo a biopsy or other types of tests.
Steps To Take
Women should start getting screened from the age of 21. You can get a Pap test to look for changes in your cervical cells that could become cancerous if left untreated. If the Pap test finds major changes in the cells of your cervix, your doctor may recommend more tests to examine for cancer. Women from 30 to 65 years of age should also get an HPV test alongside their Pap test to see they are HPV infected.
Pap Test vs. HPV Test
A Pap test checks the cervix for abnormal cell changes that, if not found and treated, can lead to cervical cancer. Your doctor takes cells from your cervix to examine under a microscope. How often you need a Pap test depends on your age and health history. Talk with your doctor about what is best for you.
An HPV test looks for HPV on a woman’s cervix. Certain types of HPV can lead to cervical cancer. Your doctor will swab the cervix for cells. An HPV test is not the same as the HPV vaccine.
Frequency of Screening for Cervical Cancer
The required frequency of your screening depends on your age and health history. Consult your doctor on what is best for you. For the majority of women, the following guidelines apply:
- If you are between ages 21 and 29, you should get a Pap test every 3 years.
- If you are between ages 30 and 64, you should get a Pap test and HPV test together every 5 years or a Pap test alone every 3 years.
- If you are 65 or older, ask your doctor if you can stop having Pap tests.
If you had a hysterectomy, you should adhere to these guidelines:
- If you no longer have a cervix because you had a hysterectomy for reasons other than cancer, you will never need a Pap test.
- If you had a hysterectomy because of abnormal cervical cells or cervical cancer, you should go for a Pap test annually until you achieve three tests with normal results.
- If you had your uterus removed but you still have a cervix, you need to undergo regular Pap tests until you are 65 years old and have had three normal Pap tests consecutively with no abnormal results in the past 10 years.
Methods of Prevention
You can reduce your risk of contracting cervical cancer by taking the following measures. These steps work best when used together. No single method can protect you from cervical cancer. Nevertheless, the best ways of preventing cervical cancer involve:
- Getting an HPV vaccine (if you are 26 or younger). Two vaccines — Cervarix and Gardasil — protect girls and young women against the types of HPV that cause most cervical cancers. The vaccines are recommended for girls who are 11 or 12 years old. The Gardasil vaccine is recommended for boys who are 11 or 12 years old. Both vaccines are licensed, safe, and effective.
- Getting regular Pap tests. Regular Pap tests help your doctor find and treat any changing cells before they turn into cancer. Women who have had the HPV vaccine still need to have regular Pap tests.
- Staying monogamous. Being monogamous means that you only have sex with each other and no one else. The best way to prevent any sexually transmitted infection (STI), including HPV, is to not have vaginal, oral, or anal sex. But, having sex with just one partner can lower your risk. That means that you only have sex with each other and no one else.
- Using condoms. Research shows that condom use can lower your risk of getting cervical cancer when used correctly and every time you have vaginal, anal, or oral sex. Protect yourself with a condom every time you have vaginal, anal, or oral sex.
What Happens During a Pap Test
All women between 21 and 65 years old are highly encouraged to go for a pap smear regularly. During this test, a doctor will use a metal or plastic speculum to widen your vagina in order to examine the vagina and the cervix. This is followed by the collection of cells and mucus from the cervical area which are then placed on a slide or in a bottle for subsequent laboratory testing.
How to Prepare for a Pap Test
You should not have a Pap test scheduled during your menstruation. In the 2 days prior to your pap spear, you
- should not rinse your vagina with water or any another fluid.
- should not use a tampon.
- should not have sex.
- should not use a birth control cream, foam, or jelly.
- should not apply any medicine or cream in your vagina.
If you are taking the HPV test along with the Pap smear, your cells collected as part of the Pap test will also be tested for HPV. Talk with your doctor, nurse, or other health care professional about whether the HPV test is right for you.
When you have a Pap test, the doctor may also perform a pelvic exam, checking your uterus, ovaries, and other organs to make sure there are no problems. There are times when your doctor may perform a pelvic exam without giving you a Pap test. Ask your doctor which tests you are having, if you are unsure.
Quest is a certified laboratory for the processing of Pap tests under the Health Promotion Board’s Screen for Life programme (CervicalScreen Singapore). If you are 21 years or older, have been sexually active before, and have not undergone a Pap test in more than 3 years, schedule an appointment with your doctor today for a Pap test done by Quest.
COLORECTAL CANCER
Overview and Definition
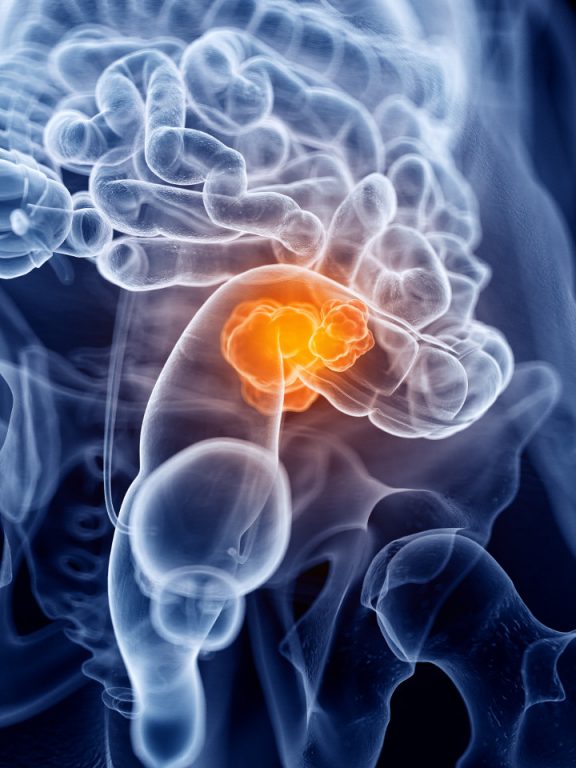
Colorectal cancer occurs when malignant cells start to form in a person’s colon or rectum. Situated in the lower part of the digestive system, the colon and rectum are components of the large intestine. During digestion, food travels from the stomach and small intestine into the colon. The colon absorbs nutrients and water from ingested food, creating in the process waste matter as stool. Stool moves from the colon into the rectum where it is stored before leaving the body.
The majority of colorectal cancers are adenocarcinomas (i.e. cancers that originate in cells that produce and release mucus and other fluids). Colorectal cancer usually starts with a growth called a polyp, which may develop on the inner wall of the colon or rectum. Some polyps may become cancerous over time. Therefore, discovering and eliminating polyps can help prevent colorectal cancer.
Symptoms
Early-stage colorectal cancer usually does not give rise to symptoms. It is therefore crucial for an individual, particularly one who is at higher risk of developing the disease, to regularly undergo the tests prescribed by a doctor. Like most diseases, early detection enhances the chances of a full recovery.
The following are the most frequently associated symptoms of colorectal cancer:
- Blood in the stool
- Rectal bleeding or cramps
- Continuous diarrhoea or constipation
- Frequent need for urgent bowel movement
- Difficulties in emptying bowel
- Feelings of discomfort in the stomach area
- Loss of appetite
- Loss of weight
- Unexplained fatigue
- Pain in the pelvis
Risk Factors
Certain risk factors can increase the likelihood of developing colorectal cancer. Below are factors known to heighten the probability of contracting colorectal cancer:
- Family history of the disease
- Those with a parent, sibling, or child with colorectal cancer
- Personal history of the disease
- Those who have had colorectal cancer, high-risk adenomas, ovarian cancer, or inflammatory bowel disease
- Age
- Persons older than 50 years of age
- Alcohol use
- Individuals who regularly consume 3 or more alcoholic beverages a day
- Cigarette smoking
- Those who smoke regularly
- Obesity
- Those who eat a high-fat diet
To help prevent the onset of colorectal cancer, it is important to try mitigating some of the risks mentioned above. For instance, making relevant lifestyle changes such as curbing alcohol consumption, eliminating the use of cigarettes, committing to regular physical activity, and maintaining a healthy Body Mass Index (BMI) can all contribute towards reducing the chances of developing colorectal cancer.
Steps to Take

Individuals 50 years and older should undergo annual screening for colorectal cancer. In Singapore, colorectal cancer is the most common cancer among males and the second most frequent cancer among females.
Generally, the screening involved for this disease entails a digital rectal exam along with the testing of stool samples for traces of blood. Where necessary, the doctor may recommend that a colonoscopy be conducted in order to carry out a comprehensive evaluation of the colon and the rectum.
Under the Health Promotion Board’s Screen for Life initiative, Quest is a certified laboratory for the processing of Faecal Immunochemical Test samples for the National Colorectal Cancer Screening Programme. If you are 50 years or older, schedule an appointment with your doctor annually for colorectal cancer screening and request for your stool specimen to be tested by Quest.
OVARIAN CANCER
Overview and Definition
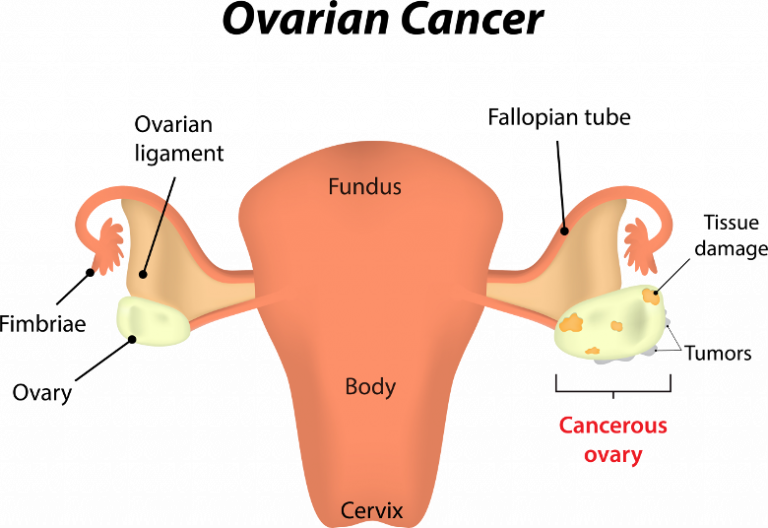
Ovarian cancer is cancer of the tissues of the ovary. An ovary is one of a pair of female reproductive glands in which ova or eggs, are produced.
Certain tumours in the ovaries can be benign, meaning they are not cancerous, while others can be malignant or cancerous. Cancers that originate in the ovaries can also spread elsewhere in the body through a process known as metastasis.
Although the majority of ovarian cancer cases occur in women over 60, this disease can also affect younger women.
High-Risk Women
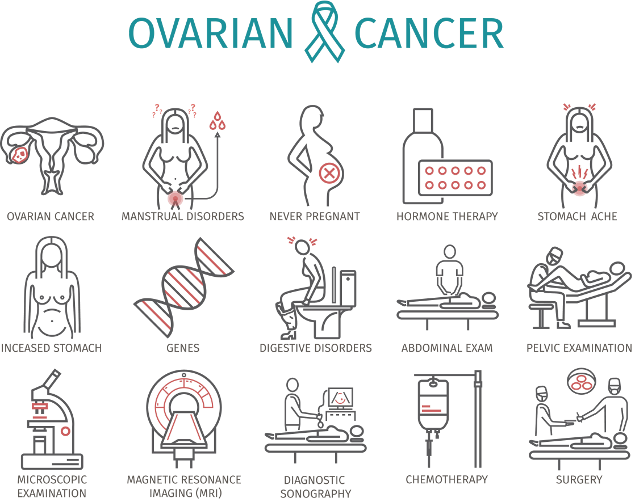
Some women are more likely to develop ovarian cancer due to their genetic make-up. Those with a harmful mutation of the BRCA1 or BRCA2 genes have a high risk of ovarian cancer. These mutations can be found by conducting a blood test. Additionally, women with a family or personal history of breast or ovarian cancer are also at higher risk of ovarian cancer.
Women who have family members from multiple generations with breast cancer or ovarian cancer should consult with their doctor to ascertain their risk of ovarian cancer. Current research shows certain measures such as surgery to remove the ovaries and the fallopian tubes may help avert ovarian cancer in high-risk women. The earlier ovarian cancer is found and treated, the higher the chance for full recovery. However, detecting ovarian cancer early is difficult because its symptoms are also those of many other diseases.
Symptoms
The following may be symptoms of ovarian cancer if they persist or worsen across time:
- Pain in the pelvis or abdomen
- Bloating in the abdomen
- Urgency in urinating
- High frequency of urination
- Constipation or diarrhea
- Feeling full quickly when eating
- Eating difficulties
- Vaginal bleeding or other abnormal discharge
- Back pain
Steps to Take
Females who experience the symptoms listed here for a prolonged period of time should consult a doctor to determine if the cause is cancer. A visit to a gynecologic oncologist may be subsequently recommended for further medical evaluation.
Women who have a high risk profile of developing ovarian cancer due to factors mentioned previously should seek medical advice on the risk they face and the best preemptive measures to take.
For those who are not at high risk of developing ovarian cancer, regular screening for the disease is not generally advised. This is due to the very real possibility of generating a false positive result from the common diagnostic methods currently employed such as blood tests, pelvic exams, and ultrasound.
PROSTATE CANCER
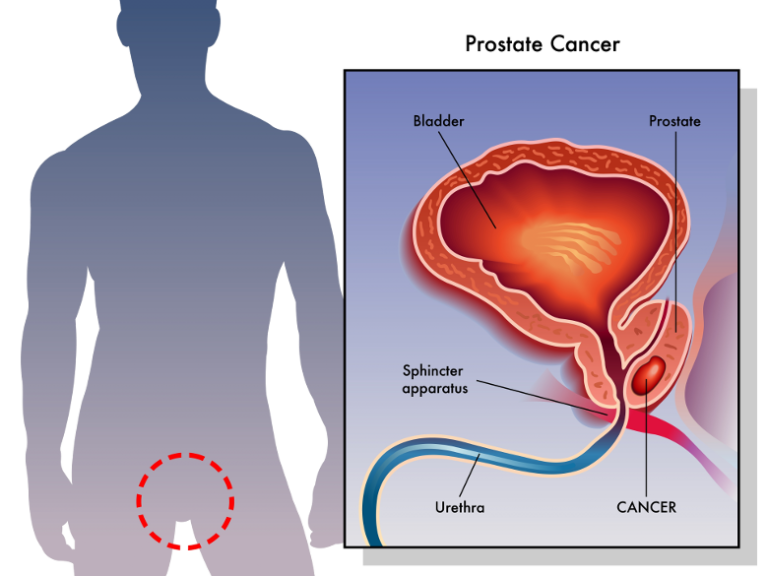
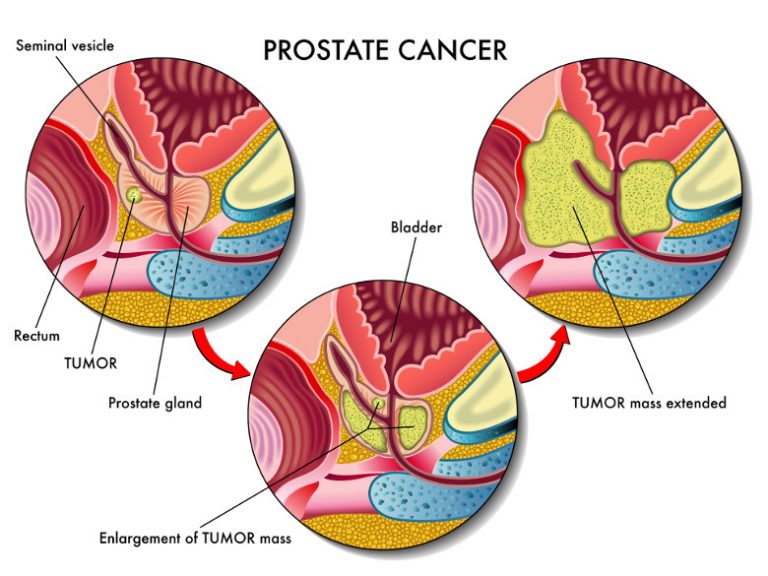
Overview and Definition
Prostate cancer occurs when cells in the tissues of the prostate grow out of control. Prostate cancer has a tendency to grow slowly vis-à-vis other cancers. Cell changes can start 10, 20, or even 30 years prior to a tumour becoming large enough to cause symptoms. The cancer cells may eventually spread, but by the time symptoms can be observed, the cancer may already be at an advanced stage.
At 50 years of age, the majority of men would not have experienced symptoms of prostate cancer, although some pre-cancerous or cancer cells may already exist. By age 80, it is not uncommon for men to have some cancer in their prostate glands. However, most of these cancers would never cause symptoms or become a serious health threat.
Symptoms
The following are the symptoms:
- Difficulties in urinating
- Frequent need to pass urine, particularly at night
- Weak or interrupted stream of urine
- Pain or burning sensation while urinating
- Blood in urine or semen
- Painful ejaculation
- Nagging pain in the back, hips, or pelvis
Prostate cancer can spread to the lymph nodes of the pelvis or even throughout the rest of the body. However, there is a tendency for prostate cancer to spread to the bones, and therefore pain in the bones, especially in the back, can be a symptom of prostate cancer at an advanced stage.
Risk Factors
Certain risk factors have been associated with prostate cancer. Although having a risk factor increases the probability of developing a particular disease, having one or more risk factors does not necessarily mean that prostate cancer is inevitable.
The risk factors for prostate cancer include:
- Age – Men who are older than 50 years
of age have a higher chance of developing prostate cancer. - Race – Certain ethnicities seem to be more predisposed to developing prostate cancer. While in the US, Asian-American men have the lowest incidence of prostate cancer, in Singapore, Chinese males account for an overwhelming majority of prostate cancer cases.
- Family history – A man whose father or brothers have had prostate cancer can be thrice as likely to develop prostate cancer compared with men without a family history of the disease. Males who have three immediate members of the family with prostate cancer have approximately ten times the risk of someone with no family history of the condition. Additionally, the younger a man’s relatives are when they developed prostate cancer, the greater is his risk for contracting the disease himself. Some research has also pointed to slightly higher risks of prostate cancer for men whose family members have a history of developing breast cancer.
- Diet – Males who regularly consume high-fat foods are more likely to develop prostate cancer later in life.
Steps to Take:
Prostate Cancer Screening
Cancer screening involves testing for cancer before any symptom arises. A screening test may help detect cancer at an early phase when it is less likely to have spread to other parts of the body, making it simpler to treat.

The most useful screening tests for cancer are those that have been proven to lower the risk of succumbing to the disease. Where prostate cancer is concerned, doctors are not entirely certain if screening lowers the risk of dying from prostate cancer. While some may feel it is best to treat any cancer discovered, including cancers found through screening, prostate cancer treatment can cause severe and permanent side effects. Some doctors are concerned that many men whose cancer is detected by screening are being treated unnecessarily.
Speak with a doctor about your risk of prostate cancer and your need for screening tests. This allows your doctor to understand your prostate concerns. You will likely be asked about possible symptoms and how they may affect you. Your medical history will also be taken so as to engage in a more holistic risk profiling.
The two major tests currently used to screen for prostate cancer are the digital rectal exam and the prostate-specific antigen test.
Digital Rectal Exam (DRE)
The DRE is a standard method for examining the prostate. Using a gloved and lubricated finger, a doctor feels the prostate from the rectum.
Lasting approximately 10-15 seconds, this exam checks for:
- Size, firmness, and texture of the prostate
- Hard areas, lumps, or growth spreading beyond the prostate
- Pain caused by touching or pressing the prostate
The DRE allows only for one side of the prostate to be felt and examined. The prostate-specific antigen test is another way of evaluating prostate health.
Prostate-Specific Antigen (PSA) Test
The PSA test is approved by the US Food and Drug Administration for assisting in the detection of prostate cancer in males 50 years and older. PSA is a protein made by prostate cells and it is normally secreted into ducts in the prostate where it helps to make semen. However, at times, PSA leaks into the blood and when this happens, it can be measured with a blood test called the PSA test. In an individual with prostate cancer, an abnormally high level of PSA gets into the blood. On its own, a high PSA blood level is not evidence of cancer. In fact, many other factors can lead to a false-positive test result. For instance, blood PSA levels are frequently elevated in men with prostatitis or benign prostatic hyperplasia (BPH). Occurrences that affect the prostate gland such as riding a bicycle or motorcycle, having a DRE, experiencing an orgasm within the past 24 hours, or undergoing a prostate biopsy or prostate surgery may all cause an increase in PSA levels.
Additionally, some prostate glands may naturally produce more PSA than others. PSA levels also rise with age. Males of certain ethnicities may also have higher PSA levels in general than men of other races. Furthermore, drugs such as finasteride and dutasteride can cause a decline in a man’s PSA level. Nevertheless, for those who have undergone prostate cancer treatment, PSA tests are often conducted periodically to look for signs of a relapse.
Despite the prevalence of the PSA test, it is yet unknown whether PSA testing to screen for prostate cancer will actually reduce a man’s risk of dying from the disease. This is due to the fact that the PSA test can help detect small tumours that do not cause symptoms. However, finding a small tumour may not necessarily lower the risk of dying from prostate cancer because some tumours found through PSA testing may grow so slowly that they are not likely to be life threatening. In fact, treating early prostate cancer can potentially lead to complications and adverse side effects.
Such being the case, researchers continue to examine the effectiveness of the PSA test in aiding doctors in distinguishing between prostate cancer and benign prostate problems. At the moment, it is generally advised that readings from PSA tests be used over time as a guide to assess if further medical follow-up is required.
PSA Test Results
PSA levels are measured in terms of the amount of PSA per volume of fluid tested. Doctors often use a value of 4 nanograms (ng) or higher per millilitre of blood as a sign that further tests, such as a prostate biopsy, are needed. Your doctor may monitor your PSA velocity, which means the rate of change in your PSA level over time. Rapid increases in PSA readings may suggest cancer. If you have a mildly elevated PSA level, you and your doctor may choose to do PSA tests on a scheduled basis and watch for any change in the PSA velocity.

